Within the past five years, West Virginia has seen the closure of three hospitals, while four other hospitals permanently closed their maternity care facilities. Currently, most women and their families must drive at least 30 minutes and up to two to three hours each way to visit their maternity care provider, to access high-risk specialty care, and to give birth. According to the Centers for Diseases Control and Prevention’s National Center for Health Statistics, West Virginia ranks seventh highest in cesarean delivery, fourth highest in preterm births, 10th highest for low birth weight, eighth highest for infant mortality, and 20th highest for maternal mortality.
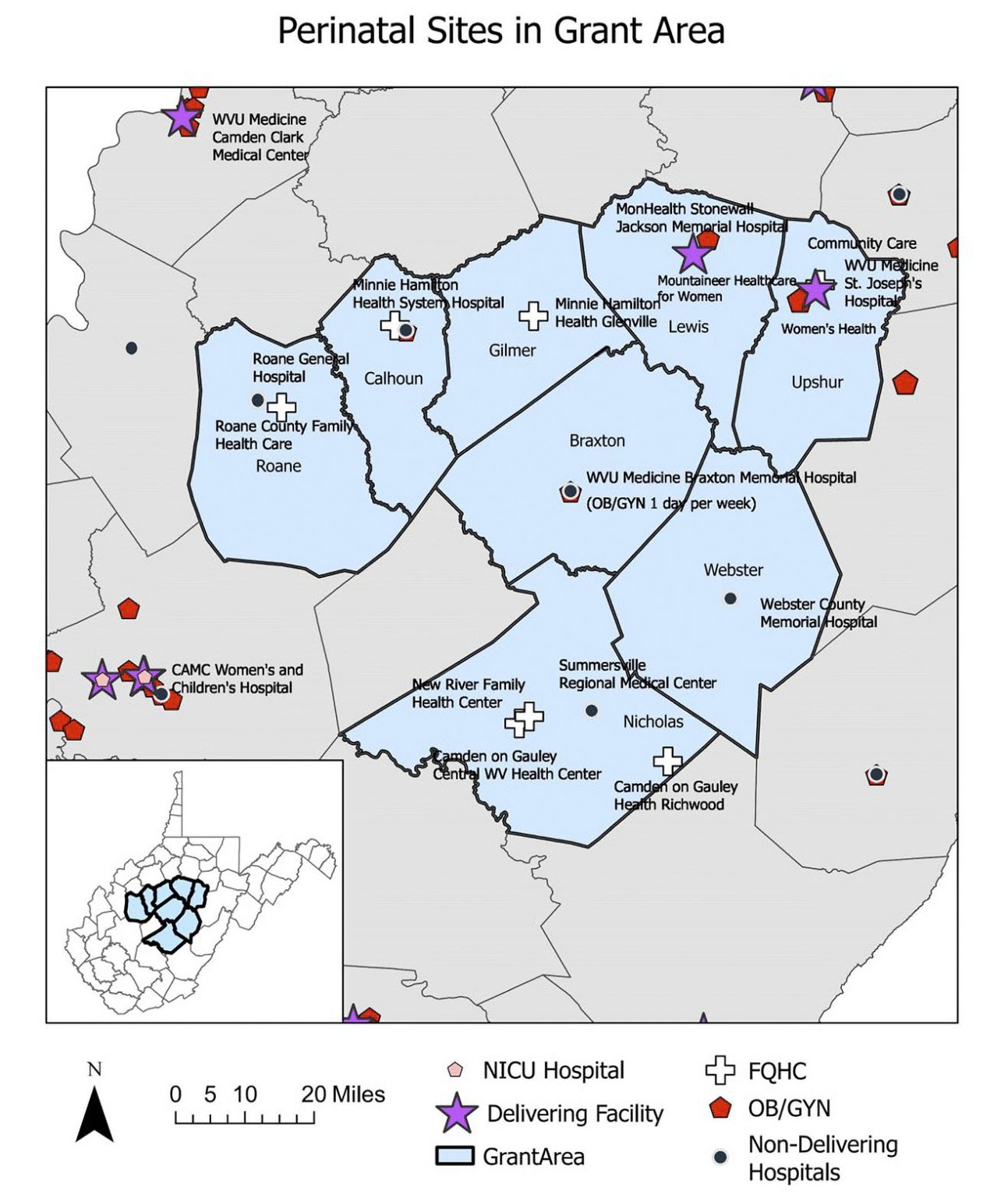
To combat these problems, the WV Rural Maternity and Obstetrics Management Strategies(RMOMS) program was developed to improve the continuity of maternity care for women from preconception through pregnancy, childbirth, and postpartum in the eight rural counties of Braxton, Calhoun, Gilmer, Lewis, Nicholas, Roane, Upshur, and Webster.
The $4 million, four-year program was funded through August 2025 by the Health Resources and Services Administration (HRSA) to address four focus areas:
Program Goals
Improve maternal and neonatal outcomes in this rural region
Develop a sustainable network approach to increase the delivery and access of preconception, pregnancy, labor and delivery, and postpartum services
Develop a safe childbirth environment with the support and access to specialty care for perinatal women and infants
Develop sustainable financing models for the provision of maternity and obstetrics care in rural hospitals and communities
The RMOMS program was launched nationally in 2019 to improve maternal health in rural areas as part of the Department of Health and Human Services’ Improving Maternal Health in America initiative. The program, which is funded by the HRSA through the Federal Office of Rural Health Policy (FORHP) and the Maternal and Child Health Bureau, uses network models to increase access to maternal and obstetrics care in rural communities and to improve health outcomes for mothers and infants.
“The opportunity to partner with the Perinatal Partnership through the RMOMS grant has lent funding to invest in the enhancement of women’s health services to close gaps for our community, as well as to improve access to services in rural communities. This collaborative allowed for reopening of women’s health services at WVU’s Summersville Regional Medical Center and creation of additional services for families currently not available, such as lactation support and childbirth education. Without having specific delivery services here, RMOMS programming has helped to empower emergency departments to prepare and care for obstetrical emergencies as well as enhancing the system of care through navigation and extension of resources. Having specific services for women and families provides the much needed emphasis and care that is required for our population, in areas laden with challenges to accessible care.”
Anita Stewart, DO
Health Officer, Nicholas County Health Department
Collaborative Members
- Braxton County Memorial Hospital
- Camden on Gauley, Camden Family Health
- Charleston Area Medical Center (CAMC) Women and Children’s Hospital
- CAMC Institute for Academic Medicine
- Community Care of West Virginia
- Minnie Hamilton Health Care Center, Inc.
- New River Health Association Inc.
- Partners in Health Network, Inc.
- Roane General Hospital
- St. Joseph Hospital of Buckhannon
- Stonewall Jackson Hospital
- Summersville Regional Medical Center
- Webster Memorial Hospital
- West Virginia Bureau for Medical Services
- WV HAPI Project: West Virginia Healthy Start/Helping Appalachian Parents and Infants Project
- West Virginia Home Visitation Program
- West Virginia Primary Care Association
“Place your hand on a map in the middle of West Virginia and you will find few hospitals and no birthing centers that offer delivery services as well as a scarcity of providers who care for pregnant women and their babies. The West Virginia RMOMS project hopes to change that.”
Shauna Lively, EdD, RN, LCCE
Director, RMOMS Project
Program Impact
The WV RMOMS program is already succeeding in its early goals, including:
1. Working with FQHCs in the target area to initiate or enhance obstetric and maternity care in five sites.
2. Providing start-up funding for telehealth, doulas and mother navigators.
3. Providing professionals with lactation education and childbirth instructor training in all 8 RMOMS counties.
4. Establishing Data, Clinical, and Financial workgroups.
